What is the third stage?
The third stage lasts from the birth of the baby to the complete birth of the placenta and membranes. It may take up to an hour to complete the third stage, but it is commonly completed within 5-15 minutes. The total time taken depends on your individual circumstances, the way third stage is managed and you and your baby’s wellbeing at birth. There are times when it is advisable to shorten this stage for the wellbeing of mother and/or baby.
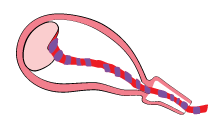
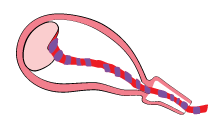
Immediately at birth, the baby has been born but is still connected to you via the umbilical cord and the placenta and membranes are still inside your uterus. The cord continues to pulsate and deliver blood to the baby from you via the placenta, although the baby does not receive much oxygen via the cord now because it is using its lungs to breathe or cry. If left unclamped, the cord naturally continues to pulsate for a few minutes before it stops altogether. During this time the baby can receive up to 100mls of blood from the mother.
If all is well, the birth partner may be involved in clamping and cutting the cord, if they prefer. The cord is about 2 cm thick and around 50 cm long. It has two arteries and one vein inside but it does not contain nerves, so the baby will not feel the cord being cut. The cord is clamped in two places and the section between the clamps is cut to finally separate the baby from the mother. When cut, the cord feels slippery, gristly and jelly-like; similar to calamari. There may be a squirt of blood from the clamped section as it is being cut. Your midwife and/or obstetrician can provide guidance on how to do this safely. The baby may have already been handed to you and your birth partner immediately at birth for a cuddle or she/he may be handed to the Neonatal Team after cord clamping and cutting for examination and resuscitation, depending on circumstances.
Birthing the placenta and membranes

The obstetrician or midwife will then turn their attention to birthing the placenta and membranes. At this time, you may start to feel or be aware of a couple of sensations once the baby has been born and your uterus starts to shrink in size.
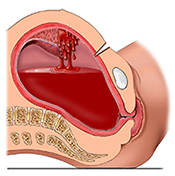
You will feel cramps in your abdomen. These are caused by your uterus contracting and becoming smaller to separate the placenta and membranes from the uterine wall. The contraction of the uterus also keeps the uterus from bleeding excessively. You may also feel fullness in the vagina and a sensation of warmth and wetness. These are caused by the placenta moving down into the vagina and a trickling of blood that accompanies the separation and birth of the placenta and membranes. The normal amount of blood loss for mothers following birth can vary greatly from a minimal amount to an average of 350 mls or more.
There are two main ways that the third stage can be managed - through active and physiological management. You can discuss these options with your obstetrician during your informed consent discussion.
Back to Top
Active management of the third stage
Many hospitals have a policy of using active management of the third stage. During active management, your obstetrician and midwife use techniques to facilitate birth of the placenta and membranes with the aim of preventing postpartum (excessive) bleeding. For active management, you can expect the following:
An injection of an oxytocic medication (usually Syntocinon) is given to the mother into a muscle or IV once the baby (or babies) is born. This increases uterine contractions that separate the placenta from the uterine wall and cause the uterus to remain firmly contracted once the placenta and membranes are birthed.
The obstetrician or midwife will usually clamp and cut the baby’s cord within seconds or minutes. The birth partner can be involved in this process.
Once it is clear the placenta and membranes have separated from the uterus, the obstetrician or midwife will simultaneously place one hand on the mother’s abdomen just above the pelvic bone to brace her uterus whilst using the other hand to pull on the cord to birth the placenta and membranes. This counter pressure on the uterus and pulling on the cord is called controlled cord traction. The mother is not required to actively push during controlled cord traction.
Once the placenta and membranes have been birthed, the obstetrician or midwife will massage the mother’s abdomen to expel any blood clots and check her uterus is well contracted to prevent postpartum haemorrhage.
The placenta and membranes are then examined for completeness.
If there is excessive continued bleeding or if you are at risk of postpartum haemorrhage, an IV infusion of Syntocinon may be commenced.
The other method of managing third stage allows placental separation and expulsion to occur spontaneously or by maternal effort. This is called physiological management. A Cochrane Review on active versus physiological management of the third stage concluded that routine active management is superior to physiological management in terms of blood loss, postpartum haemorrhage and other serious complications of the third stage of labour.
Back to Top
When is the best time to clamp and cut the cord?

The timing of cord clamping and cutting is determined by the birth circumstances. There may be an opportunity for you or your partner or support person to assist in this process if deemed appropriate.
Back to Top
Cord blood sampling and testing
Following complete birthing of the placenta and membranes, cord blood samples are routinely taken either from the cord or fetal blood vessels of the placenta, for a range of tests such as, baby’s blood group, Rhesus type, blood count and haemoglobin. If the baby has experienced fetal compromise during labour, samples may also be taken to assess blood gases and pH values.
Please check with your obstetrician and hospital about private cord blood collection or donations for cryogenic storage or use. In general, our hospital staff will not be responsible for the collection, storage or transport of such cord blood samples. Additionally, your cord blood agency must have a current agreement with the hospital to cover these arrangements.
Back to Top
Complications in the third stage - Postpartum haemorrhage
It is normal for some bleeding to occur during the third stage and immediately following the birth. A postpartum haemorrhage or PPH refers to excessive blood loss of 500 mls or more after vaginal delivery of the baby. About 1 in 10 women giving birth in Australia will experience excessive bleeding within 24 hours of giving birth.
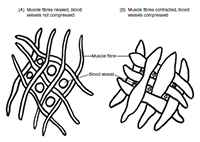
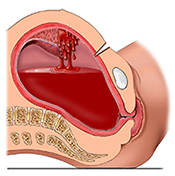
During pregnancy, at full term, the uterus sits high up near the ribs. Following childbirth and complete birthing of the placenta and membranes, the uterus sits at or just below the level of the umbilicus (belly button). The uterus should be empty and the internal walls will have come together to compress the bleeding site where the placenta was attached internally. Additionally, the powerful uterine muscle fibres form natural ligatures that remain contracted to bind the bleeding blood vessels within the uterus and further prevent excessive blood loss from the placental site.
The most common cause of PPH is that the uterus does not remain contracted, as expected, after birth. This can be caused by prolonged or very rapid labour, augmented labour, as a result of a difficult birth or when the uterus has been stretched more than usual e.g. if you had twins, extra amniotic fluid around your baby or a large baby. A low lying placenta and adherent forms of placenta can also contribute to excessive bleeding. Rarely a tear in the uterine wall or inversion of the uterus can cause PPH. In these cases the uterine muscle has become compromised and it is unable to normally and effectively stay contracted to minimise bleeding. Other causes include cervical, perineal or vaginal tears that occur as the baby is being delivered and retained placenta or membranes (which is discussed below). A rare cause of PPH is that the mother may have a blood clotting disorder.
A PPH cannot always be anticipated or prevented. However, there are a few ways that the likelihood or severity of PPH can be minimised. Research tells us that the main way, as discussed above, is to use active management of the third stage to ensure the uterus is well contracted and blood loss is minimised. Other things that can be done include:
- Antenatal history. If you have had a PPH in the past, there is a possibility of it recurring during a subsequent birth. It is important that you tell your obstetrician and midwife about this so they can prepare for this possibility. Additionally, please bring your Antenatal Record or Summary with you to the hospital so that your midwives can check your past history
- Any risk factors, such as anaemia or blood clotting disorders are identified during your antenatal testing and are corrected during the antenatal period
- Regular emptying of your urinary bladder during labour and immediately after birthing can help to minimise the possibility of PPH. The bladder sits on top of the uterus anatomically and when it is full, it can prevent the uterus from contracting down
- Adequate hydration and fluid replacement during labour. This may include the use of IV infusions if you become dehydrated
- Perineal massage and pelvic floor exercises during pregnancy, placement of warm compresses on the perineum in the second stage of labour, and maternal positioning (e.g. birthing on your hands and knees), can be used successfully to prevent or reduce the severity of perineal tears and associated PPH
- If you have had a PPH previously you may have an infusion of Syntocinon immediately after the birth to keep your uterus contracted
Your obstetrician and midwife will closely examine you and continue to routinely observe you following the birth. This involves checking that your uterus is well contracted, examining the birth canal for any tears, suturing any tears or episiotomy, and monitoring your vital signs (e.g. pulse, blood pressure, respiration). The placenta and membranes will also be examined for completeness. The blood loss at birth will be estimated. If you continue to bleed or if you show signs of compromise or shock due to blood loss, depending on the likely cause and amount of bleeding, the following actions may occur:
- Your midwife and obstetrician will explain the situation and discuss your options
- Your uterus will usually be massaged and any clots expelled
- One or more IVs may be inserted in your vein(s) and an infusion of Syntocinon and other fluids commenced
- A catheter may be inserted into your bladder to empty it
- You may need to be re-examined for the presence of any tears or retained placenta or membranes
- Blood tests may be taken
- Additional medications to contract the uterus and stop the bleeding may be given
- Depending on the amount of blood loss, you may be given oxygen
- You may be offered a blood transfusion
- Other specialists may be consulted about your care
- If the bleeding does not stop with these measures, your obstetrician may discuss the possibility of examining you under anaesthesia to better determine and treat the cause. This may involve surgical measures such as stitching, placement of a balloon into the uterus to stop the bleeding, or, in rare circumstances, performing a hysterectomy.
Once the PPH has been controlled your Maternity Team will continue to closely monitor your condition. Depending on your condition, and amount of blood loss, you may be initially cared for in the labour ward or intensive care unit (ICU).You may have more blood tests to see if your kidney function and blood clotting values are within normal ranges. Your vital signs and urine output (through a urinary catheter) and your vaginal bleeding will be closely monitored. If you had an operation your wound will be checked for any internal bleeding. You may be offered antibiotics to prevent or reduce the likelihood of infection. If a balloon was inserted into your uterus this is usually removed, through the vagina, the following day.
Following a severe PPH some mothers can be quite anaemic and very tired. Your midwives will care for you and assist you with your baby as required. The catheter in your bladder and the IV infusion will be removed once your condition improves. More information about PPH can be found in the resources section.
Back to Top
Complications in the third stage - Retained placenta (and/or membranes)
Occasionally, all or part of the placenta and/or membranes may fail to birth and be retained within the uterus. The reason for this is not always clear, but it can occur in about 1 in 15-50 births. In general, some reasons for retained placenta and/or membranes can include: if it has happened in the past, if it has either not separated or only partially separated from the wall of the uterus, if the cord snaps during birthing of the placenta and membranes, or as a result of the placenta and/or membranes becoming trapped behind the closed cervix.
If the placenta and membranes have not been birthed within an hour, if there is excessive bleeding associated with a retained placenta or part of the placenta and/or membranes are retained, there are several ways these situations can be managed. Your obstetrician and midwife will explain the situation and discuss the options with you.
- Sometimes a full bladder can prevent the placenta and membranes from birthing so you may be asked to try emptying your bladder or a urinary catheter may be inserted into your bladder
- If the cord has snapped but the placenta and membranes have separated, it may be possible for you to push the placenta and membranes out using maternal effort and positioning (e.g. squatting and pushing)
- If the third stage was initially managed physiologically, changing to active management may successfully deliver the placenta and membranes
- If there is excessive bleeding accompanying the retained placenta and membranes, the abovementioned actions for PPH may be undertaken
- Your obstetrician may discuss the possibility of removing the placenta and membranes manually. This may be performed under either regional (e.g. epidural) or general anaesthesia. You will be asked to sign a consent form and be prepared for the procedure in a similar way to other operative procedures
- Rarely, if none of these options is successful, if the placenta is very adherent (e.g. placenta accreta, increta or percreta) and there is excessive bleeding, a hysterectomy may be performed
- Sometimes, there may be smaller retained fragments of placenta or membranes that do not come to light until sometime afterwards. The first sign may be excessive bleeding and/or signs of infection (e.g. fever or chills, a tender uterus, foul smelling vaginal loss) in the postnatal ward or rarely, at home. This is called a secondary postpartum haemorrhage because it occurs 24 hours or longer after the birth. If the retained fragments are not passed spontaneously, an ultrasound to locate the retained fragments may be offered, and these may be removed surgically under anaesthesia (dilatation and curettage). Additional care for retained placental fragments that cause secondary PPH and/or infection includes antibiotics to treat any infection and medications to contract the uterus.